Hydroxychloroquine
Hydroxychloroquine (HCQ), sold under the brand name Placenyl, among others, is a drug that is sensitive to malaria chlorocaine. Other uses include treatment of rheumatoid arthritis, lupus, and porphyria catania tarda. It is taken by mouth It is being studied as a treatment for coronavirus disease 2019 (COVID-19)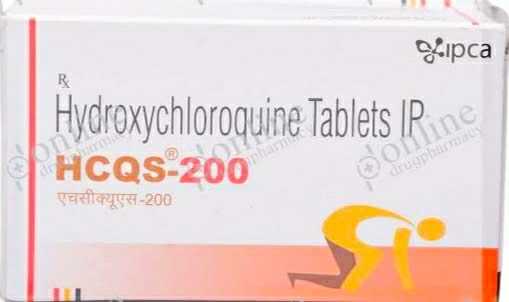 |
| hydroxychloroquine |
Common side effects include vomiting, headaches, changes in eyesight, and muscle weakness. Serious side effects may include allergic reactions Although not all risks are excluded, it remains a treatment for rheumatism during pregnancy. Hydroxy chloroquine is present in the family of drugs in the family of antimalarial and 4-aminoquinoline.
In 1955, hydroxy chloroquine was approved for medical use in the United States. It is on the World Health Organization's list of essential medicines, a safe and effective remedy for health problems. In 2017, it was the 128th most commonly prescribed drug in the United States, with more than five million prescriptions.
Medical use
Hydroxy chloroquine is used to treat systemic lupus erythematosus, rheumatoid arthritis, porphyria catania tarda, and Q fever and some types of malaria. It is considered a first-line treatment for systemic lupus erythematosus Some types of malaria, preventive strains and complex cases require different or additional medications.It is widely used for the treatment of primary soggren syndrome, but has not been shown to be effective. Hydroxychloroquine is widely used in the treatment of post-limb arthritis. Like the treatment of rheumatoid arthritis, it may have both anti-spirocytic activity and an anti-inflammatory activity.
The drug label suggests that individuals with hypersensitivity to 4-aminoquinoline supplements should not be given hydroxychloroquine. There are other barriers and caution is needed if patients have some heart attack, diabetes, or soriasis.
Side effects
The most common adverse effects are slight vomiting and sometimes abdominal pain with slight diarrhea. Even after the discontinuation of hydroxychloroquine use, dose-related retinopathy has a serious adverse effect on the eyes. Adverse effects for short-term treatment of acute malaria may include abdominal cramps, diarrhea, heart attacks, loss of appetite, headaches, vomiting and vomiting.For long-term treatment of lupus or rheumatoid arthritis, the adverse effects include acute symptoms, altered eye pigmentation, acne, anemia, hair bleaching, swelling of the mouth and eyes, swelling of the mouth, trauma, vision loss, vision loss, loss of vision. Skin color, hearing loss, bladder, wrinkles, liver problems or liver failure, hair loss diarrhea, muscle paralysis, weakness or atrophy, nightmares, soreness, reading difficulties, tinnitus, skin rashes, periodontitis, inflammation and fever Urinary discontent Hydroxychloroquine can worsen the condition of both soriasis and porphyria.
Children may be particularly vulnerable to the development of adverse effects from hydroxychlorocaine.
Eyes
The most serious side effects are retinopathy (usually with chronic use). People who take 400 mg of hydroxychloroquine or less per day are usually at risk for macular toxicity, when a person has been taking the drug for more than five years or in excess of 1,000 grams. The maximum daily safe dose for eye toxicity can be calculated from the height and weight of a person. The toxicity of macula is related to the total amount collected rather than the daily dose. Regular eye screening, even in the absence of visual symptoms, is advised to start occurring any of these risk factors.
Toxins from hydroxychloroquine appear in two different places in the eye: cornea and macula. The cornea may be affected by a specific corneal verticillata or vertex keratopathy, and this can be explained by corneal epithelial deposits. These changes have nothing to do with the dose and are usually reversed when hydroxychloroquine is discontinued.
Overdose
Serious symptoms of overdose usually occur within an hour of eating These symptoms may include sleep, vision changes, coercion, respiratory arrest, and heart problems such as ventricular fibrillation and low blood pressure. Loss of vision may be permanent Low blood potassium can also be from 1 to 2 mmol / LAbout 20% of adults have a higher risk of dying from chlorocaine, while hydroxychloroquine is estimated to be two to three times less toxic. While the amount of hydroxychlorocaine has historically been abnormal, one report states that three people died in eight cases.
Treatment recommendations include early mechanical ventilation, cardiac monitoring and activated carbon. Intravenous fluids and vasopressors may be required with epinephrine of choice. Gastric lavage can also be used Forcible treatment with benzodiazepines can be treated. Intravenous potassium chloride may be needed, yet it can be high blood potassium during illness. Dialysis appears to be useful
Interactions
The medication is transferred to breastfeeding and should be used with the care of a pregnant or nursing mother.Care should be taken when combined with liver changes with orthoglucose (solganal), cimmitidine (tagamet), or digoxin (lanoxin). The plasma concentration of HCQ penicillamine may increase which may help in the development of serious side effects. This enhances the hypoglycemic effects of insulin and oral hypoglycemic agents. Dose modifications are recommended to prevent deep hypoglycemia Antacids can reduce the absorption of HCQ Both neostigmine and pyridostigmine oppose the action of hydroxychloroquine.
Glucose-6-phosphate may have a link between hydroxychloroquine and hemolytic anemia among people with dehydrogenase deficiency, which can be reduced among African descendants.
Specifically, the FDA drug label for hydroxychloroquine lists the following interactions with the following drugs:
Digoxin (in which it may increase serum digoxin levels)
Insulin or antidiabetic drugs (where it can increase the effectiveness of a hypoglycemic treatment)
Q drugs that increase QT intervals and other arithmogenic drugs (as hydroxychlorocaine increases QT intervals and can increase the risk of ventricular arrhythmias if used simultaneously)
Mefloquine and other drugs are known to reduce concussion thresholds (co-administration with other antimalarials is known to reduce the risk of injury).
Antipileptics (concurrent use may worsen antipileptic activity)
Methotrexate (combined use may increase the incidence of uneducated and side effects)
Cyclosporine (where it was reported that a plasma cyclosporine level was used together).
Pharmacology
Hydroxychloroquine has the same pharmacokinetics as chlorocaine, rapid gastroenteretic absorption and destruction by the kidneys. Cytochrome P450 enzymes (CYP2D6, 2C8, 3A4 and 3A5) metabolize hydroxychloroquine to N-desethylhydroxychloroquine.
Pharmacodynamics
Antimalarials are lipophilic weak bases and easily pass plasma membranes. The free base forms in the lysosome (acid cytoplasmic vesicle) and is then protonated, resulting in a concentration 1000 times higher in the lysosome culture than in the media. This raises the pH of the lysozyme from four to six Changes in pH create barriers to lysosomal acid processes that reduce the effects of protolysis. High pH within the lysosome reduces the secretion of intracellular processing, glycosylation and protein, which has many immunological and non-immunological consequences. These effects are believed to be due to the activity of immune cells such as chemotaxis, phagocytosis, and superoxide production by neutrophils. HCQ is a weak depressive base that can pass through lipid cell membranes and concentrate in large amounts of acid in cytoplasmic vesicles. High-pH peptide loading of these vesicles in macrophage or other antigen-presenting cells and / or the subsequent processing and transport of the peptide-MHC complex in the department for autogenic peptide synthesis with second-class MHC molecules.
Mechanics of work
Hydroxychloroquine lysosomal pH increases in antigen-presenting cells. In inflammatory conditions, it blocks receptors such as tolls on plasmacoid dendritic cells (PDCs). The cells mature and present antigen in T cells Hydroxychlorocaine, by reducing TLR signaling, reduces the activity and inflammation of dendritic cells.In 2003, a novel approach was described in which receptors (TLRs) such as hydroxychloroquine tolls prevented the excitation of 9 family receptors. TLRs are cellular receptors for microbial products that cause inflammatory reactions through the activation of the built-in defense system.
Like other quinoline anti-malarial drugs, quinine's anti-malarial technique has not been completely resolved. The most acceptable model is based on hydrochlorocaine and includes the restriction of hemozoin biocrystallization, which facilitates the synthesis of cytotoxic heme. Free cytotoxic hemp accumulates in parasites and causes death.
Price
The wholesale price in developing countries has been around $ 4.65 since 2015, when it was used for rheumatoid arthritis or lupus. The wholesale price of a month of treatment in the United States is about $ 25 by 2020. In the United States, the amount is about £ 5.15 per person for healthcarehydroxychloroquine Brand name
It is often sold as a sulfate salt known as hydroxychloroquine sulfate. 200 mg of sulfate is equal to 155 mg of salt baseThe brand names of hydroxychloroquine include Plecnyl, Hydroquin, Axemal (in India), Dolquin, Queensil, Quinoric.
Regulatory approval
On March 17, 2020, the AIFA Scientific Technical Commission of the Italian Medical Agency issued a favorable opinion, including the off-label use of chlorocaine and hydroxychloroquine for the treatment of COVID-19.In the United States, several state pharmaceutical boards have reported that some doctors and dentists are prescribing hydroxychlorocaine for themselves, family members and staff, and prescription drugs for chlorocaine. Due to the hospital's use for critically ill COVID-19 patients, there has been a sudden shortage of prescriptions for demand spikes and prophylaxis; Doctors have expressed concern that patients who have taken hydroxychloroquine for other approved indications, such as lupus and rheumatoid arthritis, will be unable to afford the necessary medication.
On March 28, 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authority (EUA) for the distribution and use of hydroxychloroquine sulfate and chlorocaine phosphate products to the Strategic National Stockpile (SNS). With COVID-19



1 Comments
While it may be time to retire those little helpers from yesterday, there are still those pesky winter things that can take us out from under those warm blankets--coughing, fevers, etc. We’ve rounded up the information about hydroxychloroquine as well as tips from those in the know that may help bring some relief back into your life this season.